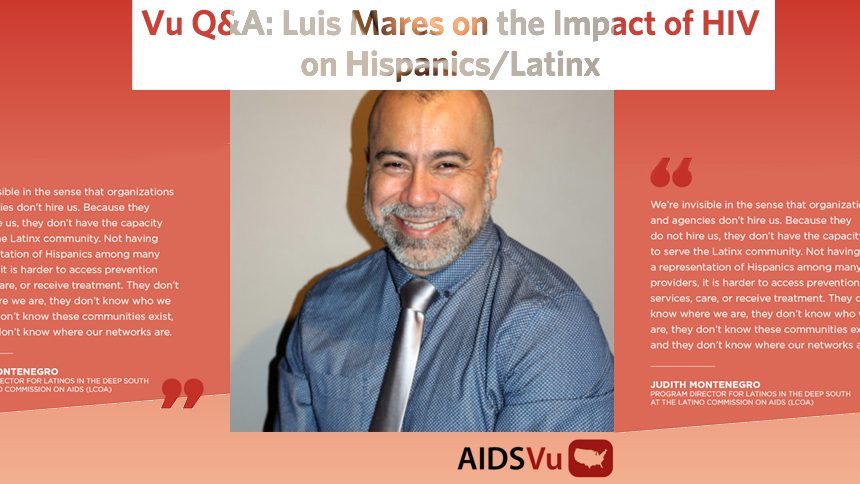
Luis (Beto) Mares, LMSW, National Community Mobilization Director for Latino Commission On AIDS (LCOA)
Q: You have been organizing the Latino Commission on AIDS (LCOA)’s awareness day activities for a little over a year and working in the HIV field for even longer. What motivated you to get involved in this work?
I started working at the Latino Commission on AIDS over a year ago but previously worked for 14 years at a YMCA Transitional Housing Program for homeless people living with HIV and AIDS in New York City. I was hired as the Healthcare Coordinator and then I became the Program Director. That began my formal experience working with people living with HIV in the U.S. Being from Peru, I always tended to have jobs that helped people, I was a fireman and a physician. When I was living in Peru and still a student, I saw a few of the first HIV cases in Lima, Peru. I felt like I needed to get involved because it was my community being impacted by this disease and I had a personal and career focus on helping people.
When I moved to New York, I faced a different reality. It became more real for me when several of my friends in New York were either diagnosed with HIV or were affected somehow by HIV. At the YMCA I began to learn about the stigma, homophobia, lack of services, communication issues, homelessness, drug use, and other factors that people with HIV live with. After several years in that job, I began to feel like I could do more, so I went back to grad school at NYU and completed a Master’s program in Social Work.
I believe that it is important to create awareness for HIV for the community-at-large, even more so now that we have the tools to decrease the number of new cases, and the newest medications can really help people living with HIV to live longer and healthier lives, as well as to not transmit the virus to other people. I also believe we need to focus on other factors around HIV, not just the medications and the prevention techniques, but also all the other determinants of health that affect the access to services to those living with and most at risk for HIV.

Q: In 2016, Hispanics/Latinx accounted for a quarter of all new HIV diagnoses, despite only accounting for 16% of the U.S. population. Additionally, while new diagnoses have been decreasing for all races/ethnicities, Hispanic/Latino men who have sex with men (MSM) have seen the smallest decrease. In your opinion, what is driving the disproportionate impact of HIV on Hispanics/Latinx?
It’s really, really worrying. We must focus on the impact of HIV in our community. We have to remember that a big proportion of the new HIV diagnoses among Latinos are among new immigrants to this country. Many of those newly diagnosed are undocumented. Therefore, they have limited or no access to any type of health services, including HIV services. Even if they are here legally, they may not have health insurance, and without insurance, they don’t have access to the type of health services they need to be tested and treated for HIV. Language is also a barrier. Many service providers don’t have the cultural and/or linguistic competency to serve Spanish-speaking communities, and there is a real need for these services.
Within the Latino community, there’s a lack of awareness and many misconceptions around HIV. Many Latinos are not properly educated about how HIV is transmitted and how it can be prevented. Testing is also low within the Latino community, meaning almost 2 in every 10 Latinos living with HIV do not know their status and as we know, being undiagnosed for a longer time increases the chances of transmission. In the Latino community, there is a lot of stigma around sex, which may also contribute to the low rates of testing. Sex is something that Latinos do not talk about much. It is something we are embarrassed about, something taboo, and therefore it makes it difficult to talk about techniques of prevention with children, young people, and among partners. Stigma also impacts many Latino communities such as homophobia and transphobia. This puts individuals that contract HIV at a higher risk to progress to AIDS and get complications. Many Latino men who have sex with men do not identify openly as gay or bisexual because of the stigma related to it, and they are forced to choose between their culture and their sexuality. For those who remain within their culture, hiding their sexuality makes it more difficult to take the test or use prevention methods openly. All these factors combined definitely impact the number of new diagnoses of HIV among Latinos.
Q: AIDSVu and HepVu visualize data on HIV and Hepatitis C across the U.S. and the impact on Hispanic/Latinx populations. How does visualizing these epidemics help support your work with community mobilization?
They say that an image is always better than a thousand words, and AIDSVu and HepVu do a great job of showing the impact of the epidemics. They do this not just through a map where you can see where the epidemics are concentrated, but also through infographics that are very useful in educating people on the impact of the epidemic on Latinos and other groups in different parts of the country. It is important for us to know what areas are most impacted by these epidemics, so we can concentrate our efforts in coordination with partners in these areas.
Q: In honor of National Latinx AIDS Awareness Day coming up on October 15, what is your message to the Latinx community?
My message would be that Latinos continue to be disproportionately impacted by this epidemic in the United States, we should concentrate our efforts in creating awareness about the importance of HIV testing and using preventive techniques.
We have the tools now to fight this epidemic. We should use them, get tested frequently, and consider PrEP as a preventive method, as well as continue using condoms to prevent not just HIV, but other sexually transmitted infections.
Ending HIV is everyone’s job, and only working together will we be able to decrease the number of new infections.
Source: This article was originally published at www.aidsvu.org